Rejected Emergencies
The narrative has become… you must have been rich enough to contract the disease, wealthy enough to be tested and popular enough to be noticed you died.
We are in troubled times.

COVID19 transmission is pushing the boundaries of many health systems around the world. Governments are announcing flip flop policies on what is expected of their citizens.
Go to school! No, go back home.
Plans of easing the lockdown are quickly being reversed as confirmed cases and the death toll rises.
Doctors, nurses and laboratory operators have been arrested for calling for strike action amidst requests for special pay packages to battle the virus as hundreds of people are showing up to the hospitals with mild to chronic level symptoms of COVID19.
COVID19 is the cause of economic downturns, job losses, business lockdown, home offices and social interaction, engagement & distancing. Developed nations are admitting that things are getting out of control. The developing nations like Nigeria are copying failing health policy and measures that are a misfit for the population and resources available.
Every infected individual has a story on how things got this bad, 74% of infected cases in Nigeria don’t know how they got the virus. No idea of who they contracted the disease from and how they have passed on the virus. Others with underlying top medical conditions such as heart disease, respiratory disease, cancer, diabetes and more are attempting to stay away from other living things.
Over 11.6 million confirmed cases and half a million dead cannot be a falsified story.
This is how the world is now.
A place to look for how to stay away from people to stay alive.
A place to look for how to stay away from people to stay alive.
The Brazilian President Jair Bolsonaro had claimed COVID19 was a “little flu” and started off a no mask advocacy against his governors. He appeared in videos and pictures with little regard for the pandemic.
He eventually had a change of heart and was low on luck.
Around the corner is a new trend.
According to the NY Times, a woman visited ‘8 Hospitals in 15 Hours: A Pregnant Woman’s Crisis in the Pandemic. Her baby was coming, and her complications were growing more dangerous. But nowhere would take her — an increasingly common story as India’s health care system buckles under pressure.’
The trend of rejection of emergencies due to facilities is growing as some are not even taking in new patients.
Who treats what?
A journalist wrote:
‘Testing in the FCT (Abuja, Nigeria) is a scam. I say it without mincing words based on my experience. … Some of our colleagues who know me will well admit that I have been seriously under the weather since Monday. My management advised that I go for a test for fear I had been exposed.
Tomorrow makes it one week... after driving around the town, nowhere to test. I resulted to phone calls using connections from fellow colleagues. Up till today, we will come today… we will come tomorrow...Its one week now and God be praised, the worst is over, yet I cannot be tested.
I imagine what will happen to those who don't know anybody and they are genuinely infected, this is so disappointing.
Whoever is responsible, NCDC or FCT, this is a big shame’
The tales of test, transmission and treatment linger on what COVID19 has become to Nigerians. The narrative has become… you must have been rich enough to contract the disease, wealthy enough to be tested and popular enough to be noticed you died.
Dealing with medical professions
The Nigerian Medical Associations with over 35,000 doctors had earlier complained of complacency on the side of the government in drawing up an informed plan with stakeholders to tackle the virus during its wake in Nigeria. A critical stage of who treats what started off when the National Association of Resident Doctors (NARD) went on strike action to push home for demands on health insurance and improved hazard allowances.
Facing off with COVID19 for hours during wards round should not be taken lightly.
‘Our health insurance is N5,000, what can anyone treat if exposed to the virus’ says the 1st Vice President of NARD, Dr Julian Ojeba.
‘It takes about 400,000 Naira to treat hepatitis if infected, what will it take to treat COVID19? We cannot ask our doctors to turn away patients and people coming to the hospital for treatment of symptoms of malaria and by extension maybe COVID19.’

In Nigeria, over 800 doctors (June 2020) were infected as they were exposed and contracted the disease from patients. A mismatch of the number of doctors able and available to treat cases in Nigeria is alarming. The plight of doctors is meshed up in hazard allowances and terrible working conditions described by NARD President, Dr Aliyu Sokomba as “grossly inadequate” supply of mask, gloves and other PPE’s is the trend.
The government made an attempt to consolidate its position by appealing that the times are hard to desert people at a time they are in dire need for the services of the highly esteemed professions.
Ebonyi state in Nigeria is asking its health workers to undergo a COVID19 test to ascertain they are healthy enough to treat people. One can only imagine if a doctor or nurse with COVID19 is treating hundreds of people daily.
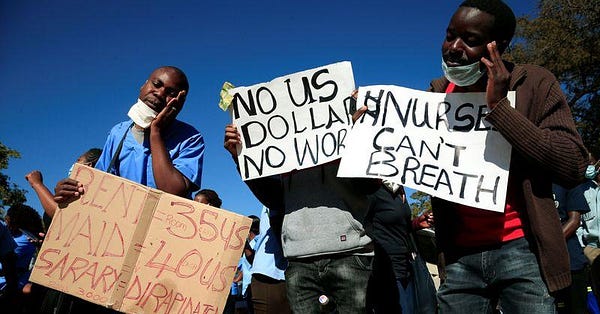
The appeal that all hands must be on deck to fight off disease is becoming emotionlessly captivating as many hands in gloves are withdrawing from the process. Zimbabwe, a southern African country went rogue by arresting nurses for the planned strike action asking for improved allowances.
The Nurses Associations in Harare, Zimbabwe say "If ever we were in doubt about the nature of the government’s response to our genuine plight, this is the clearest evidence we could have got".
Health transactions during treatment?
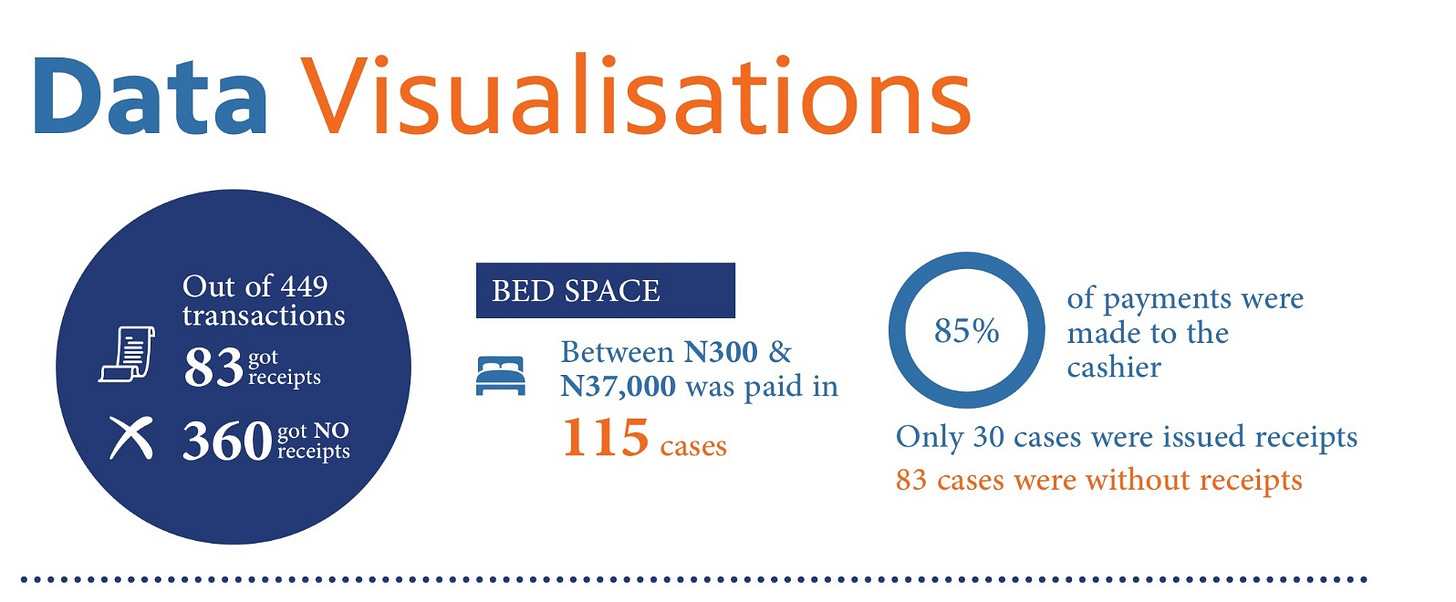
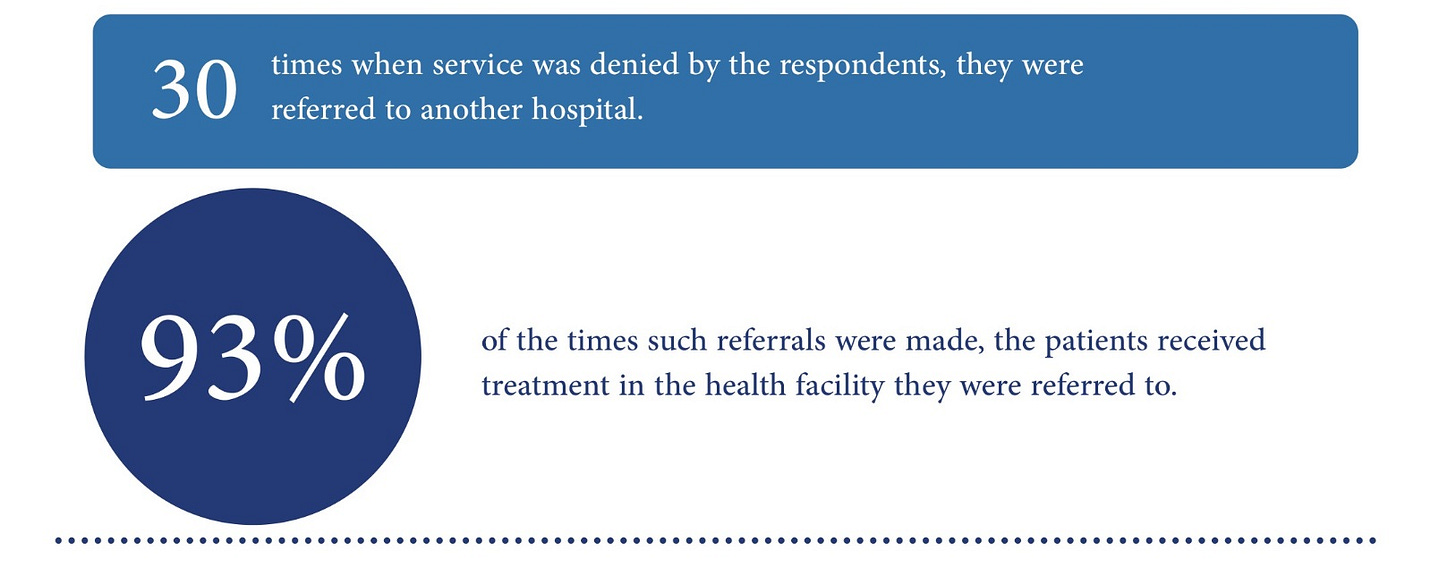
A survey of transactions for health services carried out by a team of researches at dataphyte provides a new reference point, Corruption Victimization Survey.
Some quick visuals

Patient Dumping Begins
As COVID19 raged across Europe, many medical practitioners found themselves pumping doses of drugs into patients admitted to corridors just to keep them alive until detailed consultation can be done.
Speed is one of the most powerful components of dealing with an emergency.
For the very organised health care systems, disarray of procedures had emerged. Many hospital premises are like chambers for disease spread.
Out of hospital treatment is next to impossible, even the Brice de le Vigne, Head of Médecins Sans Frontières, MSF’s COVID-19 task force says ‘our teams, we have been pushed to find solutions beyond our usual way of operating to be able to continue caring for patients. Our surge capacity during emergencies is normally built on being able to move specialist experienced staff and medical supplies around the world at a moment’s notice.”
A simultaneous relationship between the fear of going to the hospital and wondering if complications from staying away from the hospital would arise is a vital and yet complex decision for people with emergencies.
A thread for many months to come will see more die from complications of COVD19 and health complications due to COVID19 due to failing health.